More Information
• When was the last time you had an HIV test and what was the result of that test?
The only way to know for sure if you have HIV is to get tested. Before having sex for the first time, you and your partner may want to get tested for HIV and learn the results. Be aware that there’s a window period, which is the time between when a person gets HIV and when most HIV tests will show that a person has it. If you have sex before you learn your test results, using a condom the right way every time you have sex can lower your risk for getting or transmitting HIV.
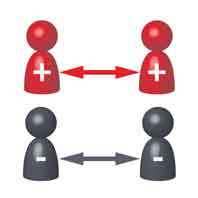
If you learn that you have HIV, the most important thing you can do is to take antiretroviral therapy (ART) as prescribed. ART is recommended for all people with HIV, regardless of how long they’ve had the virus or how healthy they are. ART can reduce the amount of HIV (viral load) in your blood. Taking ART as prescribed can make your viral load so low that a test can’t detect it. This is called an undetectable viral load. If you keep an undetectable viral load , you can stay healthy for many years and will not transmit HIV through sex.
• Are you living with HIV and on treatment?
If you have HIV, the most important thing you can do is be on treatment (ART). If you take ART as prescribed and keep an undetectable viral load, you can stay healthy and will not transmit HIV through sex. If you’re taking ART, follow your health care provider’s advice. Visit your health care provider regularly and take your medicine as prescribed. This will give you the greatest chance of having an undetectable viral load. Even if you have undetectable viral load, you or your sex partner may want to use additional prevention options. Using a condom the right way every time you have sex can protect you from other STDs. Using condoms or having your partner take medicine as prescribed to prevent HIV (called pre-exposure prophylaxis or PrEP) can provide added peace of mind. Also consider using additional prevention methods if you
- Are unsure, for any reason, that you have an undetectable viral load
- Have a higher viral load (200 copies/ml of blood or greater)
- Have trouble taking HIV medicine regularly
- Missed some doses since your last viral load test
- Have stopped taking HIV medicine or may do so in the future
• If your partner has HIV, encourage your partner to take ART too.
If you’re HIV-negative and have a partner with HIV who is taking ART as prescribed, they will not transmit HIV to you through sex as long as they keep an undetectable viral load. Even if your partner has an undetectable viral load, you or your sex partner may want to use additional prevention options. Using a condom the right way every time you have sex can protect you from other STDs. Using condoms or taking medicine as prescribed to prevent HIV (called pre-exposure prophylaxis or PrEP) can provide added peace of mind. Also consider using additional prevention methods if you are unsure, for any reason, that your partner has an undetectable viral load.
• You and your partner should learn about all the available prevention options and make the decisions that are right for both of you.
If you’re not taking PrEP, you can take post-exposure prophylaxis (PEP) if you have a recent possible exposure to HIV. For PEP to work, you must start it as soon as possible, and always within 72 hours of a recent possible exposure.
• How many other sex partners do you currently have?
Having multiple sex partners increases your risk for HIV. The more sexual partners you have in your lifetime, the more likely you are to have a sex partner with HIV who does not know their status, is not taking medicine to treat HIV, and/or does not have an undetectable viral load. It also increases the chances that you have a partner who has another STD.
• Do you have any other STDs?
Having other STDs increases your risk for getting or transmitting HIV.
• Do you use needles or syringes to inject drugs?
Sharing needles, syringes, or other drug injection equipment (for example, cookers) increases your risk for getting or transmitting HIV.


















 PrEP can be pills or shots that reduce your chances of getting HIV from sex or injection drug use. Studies have shown that PrEP is highly effective for preventing HIV if it’s taken as prescribed. PrEP is much less effective when it isn't taken consistently.
PrEP can be pills or shots that reduce your chances of getting HIV from sex or injection drug use. Studies have shown that PrEP is highly effective for preventing HIV if it’s taken as prescribed. PrEP is much less effective when it isn't taken consistently. 
 If you’re HIV-negative or don’t know your HIV status and think you have recently been exposed to HIV during sex (e.g., if the condom breaks) or through
If you’re HIV-negative or don’t know your HIV status and think you have recently been exposed to HIV during sex (e.g., if the condom breaks) or through  Use a condom the right way every time you have sex:
Use a condom the right way every time you have sex: